Deadly heat is killing Americans: A decade of inaction on climate puts lives at risk.

Heat now causes more deaths than hurricanes, tornadoes or floods in most years, creating a new public health threat. An investigation reveals why the CDC’s prevention efforts have faltered.
This story is co-published with Columbia Journalism Investigations, the Center for Public Integrity and Covering Climate Now. Read the full investigation here.
Charlie Rhodes lived alone on a tree-sparse street with sunburned lawns just outside Phoenix, Arizona. At 61, the army veteran’s main connection to the world was Facebook; often, he posted several times a day. But as a heatwave blanketed the region in June 2016 – leading to temperatures among the highest ever recorded – his posts stopped. Three weeks later, a pile of unopened mail outside his door prompted a call to police.
When officers arrived, they were overcome by the odor of rotting garbage, worsened by the still-searing heat. Inside the home, they found the air conditioner broken and its thermometer reading 99F. Rhodes lay dead in the bedroom, his body decomposing. The cause, his autopsy shows: “Complications of environmental heat exposure.”
Yearly heat-related deaths have more than doubled in Arizona in the last decade to 283. Across the country, heat caused at least 10,000 deaths between 1999 and 2016 – more than hurricanes, tornadoes or floods in most years.
Scientists link the warming planet to a rise in dangerous heat in the US, as well as the spread of infectious diseases and other health conditions. Federal research predicts heatstroke and similar illnesses will claim tens of thousands of American lives each year by the end of the century. Already, higher temperatures pose lethal risks: the five warmest years nationwide have all occurred since 2006. In the last six decades, the number of annual heatwaves in 50 US cities has, on average, tripled. In contrast to a viral pandemic, this is a quiet, insidious threat with no end point.
A decade of missed opportunities
The US Centers for Disease Control and Prevention (CDC) is charged with helping cities and states adapt to threats like extreme heat. Its climate program, created more than 10 years ago, is the federal government’s only sustained effort to bolster state and local health departments’ fight against global warming. But the program has been hampered by a decade of underfunding, limited expertise and political resistance, Columbia Journalism Investigations and the Center for Public Integrity found.
Interviews with more than 100 people and a review of hundreds of pages of government records show the Obama administration, while pushing measures to combat climate change, missed opportunities to expand the program. Under Donald Trump, officials have tried to eliminate it.
The tepid federal response has left state and local health workers ill-equipped to act, exposing communities to underappreciated threats that will only get worse.
Arizona’s health department receives around $200,000 a year to fund its climate team. But for a state with 7 million people – including a growing number of isolated, older residents like Rhodes – experts say it’s not enough to pay for research and, most importantly, action.
Rhodes, a once gregarious jokester who cut himself off from family and friends after the loss of his job and father, had devised a method to handle the heat: he covered his windows with aluminum foil and ran the air conditioner in his bedroom. But as the temperature hit 120F near his home, no one checked on him.
Asked what the program has done to prevent people like Rhodes from dying of heat, the Arizona health department spokesperson Holly Poynter said its advisories on the hottest days include a sentence encouraging people to check on at-risk friends, family and neighbors twice a day. “Heat-related deaths are preventable,” she said, “and continued work is needed due to increasing vulnerable populations within the state.”
The CDC defended its efforts on climate change, saying its program has assisted health departments successfully for years. “We’re proud of the work that our program is doing,” said Patrick Breysse, who heads the agency’s environmental health center and oversees its climate activities. “We’re excited about the leadership role we play.”

Some CDC-aided health departments lead the nation in heat illness prevention. San Francisco’s climate program helped devise heat emergency response plans and mapped vulnerable city neighborhoods. Now, officials use these maps to encourage neighbors to check on each other. Climate programs elsewhere helped change the threshold for heat advisories from 100F to 95F after finding residents get sick at lower temperatures.
Yet many departments funded by the CDC are struggling to fulfill the program’s mission, according to government and academic reports and interviews with state and local health workers.
In North Carolina, program employees asked their CDC counterparts for guidance and expertise to identify the state’s climate health threats. Records show the agency failed to provide the assistance it promised early on. After nearly a decade of research, health workers only recently began reaching out to the most vulnerable residents.
In Florida, heat-related hospitalizations are on the rise. But health officials there barred the state climate team from publicly acknowledging global warming’s link to heat. Then, with the CDC’s imprimatur, they evicted the program from the health department.
Most of the country’s 3,000 state and local health departments, meanwhile, get no such funding. They’re on their own to figure out what to do and how to pay for it.

A slow start
Federal officials have known for decades that climate change poses a public health crisis. In 1989, the US Environmental Protection Agency issued a 100-page report on how global warming could affect human health. It urged public health agencies to fund research on extreme heat and provide health departments with “trained professionals”. By 2000, the US released its first recurring assessment of the changing climate’s impacts. Again, it called for “investments in advancing the public health infrastructure”.
Five years later, Dr Howard Frumkin, a veteran epidemiologist hired to run CDC’s environmental health center, brought the nation’s leading public health agency into the battle against climate change. “We knew that the climate was warming,” said Frumkin, who viewed the CDC as “past the point where we needed to be stepping up”.
Obama’s mixed climate record
In 2009 – then the second-hottest year on record – Frumkin seized an opportunity to expand the CDC’s climate efforts. That February, he testified before a congressional committee about challenges brought by global warming. Health departments, he said, require climate and health training and data to plan for impacts. “CDC has in place many of the building blocks,” he told the committee, but it needed to assemble them into a serious effort.
A month later, a Democratic-led Congress gave the CDC $7.5m for its climate program, to be renewed yearly with congressional approval. The new initiative seeded climate and health activities in 10 health departments. Frumkin hoped it would eventually expand to all 50 states.
Shortly after Congress funded the program, Dr Thomas Frieden, then the newlyappointed CDC director, introduced his “winnable battles” – seven health initiatives that his agency prioritized. Climate was not among them. Most of those programs – nutrition, food safety – received an annual $50m to $700m by the end of his eight-year tenure. The climate program, by contrast, never exceeded $10m. In 2013, the CDC recommended reducing that budget.
As the CDC’s director, Frieden rarely used his bully pulpit to address threats posed by the warming planet. During a 20-minute keynote speech at a national environmental health conference, he discussed the topic for 13 seconds. A 2015 report by the Government Accountability Office, a congressional watchdog, criticized the CDC for failing to provide leadership on the issue.
As heat waves increase, nights are getting hotter
In cities across the U.S., heat wave seasons are getting longer and more nights are hitting temperatures that put them in heat-wave territory. Scientists say climate change and urbanization both contribute to this nighttime trend.
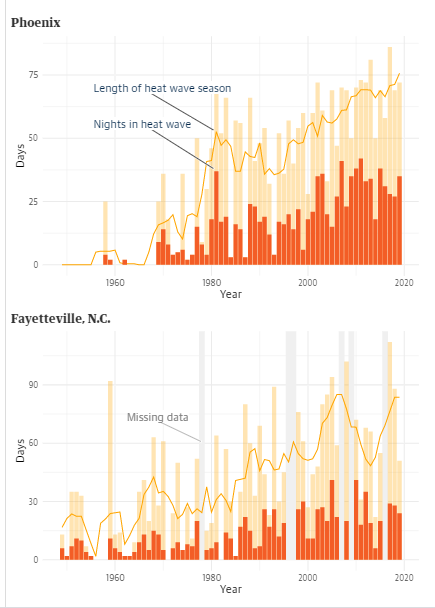
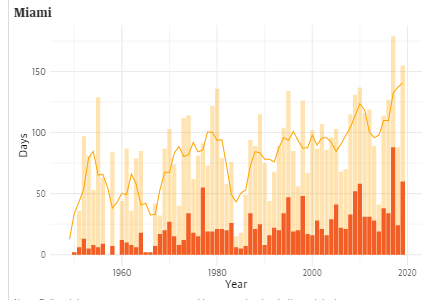
Note: Daily minimum temperatures were used because scientists believe nighttime temperatures may have more impact on human health. Heat waves are two or more consecutive days with minimum daily temperatures at or above the 85th percentile of July and August minimum temperatures, using 1961-1990 as a base period and calculated separately for each location — similar to a method used by a scientific study. The heat wave season is defined as the number of days between the first and last heat wave of each year. In Fayetteville, some years contained missing data; those years were omitted from the analysis.
Source: Analysis of NOAA National Climatic Data Center data. Credit: Elisabeth Gawthrop, Columbia Journalism Investigations / Center for Public Integrity.
Arizona health officials still don’t know why more residents like Moore are dying or how best to protect them. Temperatures are rising in the state, but the hottest summers don’t always match the highest death tolls. The Arizona State University researcher David Hondula, who works with the state’s climate team, contributed to a study ruling out temperature as the only reason. Other factors such as homelessness and substance abuse may play a role, he said, but the climate program doesn’t have money to keep studying the problem.
“If additional funding existed, we could really dive in to answer this question,” Hondula said. Instead, the limited CDC money – budgeted before the spike in deaths – supports awareness campaigns in poorer areas such as Yuma county.
Many Arizona cities offer cooling centers – air-conditioned libraries, churches and other shelters – for residents to escape the heat. Moore and Rhodes both had access to a vehicle. Cooling centers were nearby. Health workers are now surveying residents who visit cooling centers, but they say it takes money to determine why so many others don’t.
Ivan Moore, who grew up hearing about heat death victims on the radio, blames himself for what happened to his father. “I should have had someone check on him sooner,” Ivan said, even though less than 36 hours had passed between Gene’s last email to his family and when police found him. “He had quite a few years left on him.”
A worker collapse at a sweltering factory
In North Carolina, the CDC-funded program has helped enable what health department spokesperson Kelly Haight Connor described in an email as “the substantial growth in climate and health adaptation”. Even so, documents show the climate team ran into roadblocks almost as soon as it tried to evaluate the state’s preparedness for climate change. It was still seeking the agency’s assistance when, in 2015, it completed an analysis showing heat-related mortality would increase over the coming decade.
On 22 June that year, Sherion Winfrey, 63, had just returned to work after vacation and had nine days before she was due to retire. For nearly 40 years, she worked at the same oil- and air-filter factory in Fayetteville, North Carolina, a city in the Sandhills. She’d learned to pack frozen water bottles in a cooler to keep herself refreshed on the hot assembly line. But that day, as the temperature outside hit 96F, she collapsed during her shift. Rushed to a hospital, she died early that afternoon.
A state inspection of the factory the next day found that heat from industrial ovens and the metal walls and roof of the un-air-conditioned production line raised the indoor heat index – a combined measure of temperature and humidity – to over 106F and into the Occupational Safety and Health department’s “danger” heat classification. The inspector recommended the factory allow employees time to acclimate to the heat after an absence. But the investigation into Winfrey’s death ended after a medical examiner found that Winfrey suffered “a fatal pulmonary embolism and did not die from exposure to extreme temperatures”. Recent research suggests this type of blood clotting may be brought on by daily temperature swings.
Danny Muhammad, Winfrey’s son, has no doubt heat contributed to her death. Winfrey complained to family about the factory’s stifling environment. “The heat index was out of this world that day,” Muhammad said. It was the ninth consecutive day that temperatures had reached at least 94F – seven degrees hotter than the June average. Winfrey’s family filed a wrongful death lawsuit in 2017 against the factory, citing extreme indoor temperatures as the cause of her death, but the case was later dismissed. A spokesperson for the factory declined to comment.
It took another three years after Winfrey’s death for the North Carolina program’s heat education efforts to begin in four Sandhills counties – and not where she had lived.
Budget cuts and self-censorship under Trump
In the years since the Trump administration took over, the political pressure hampering some of the CDC climate program’s grantees has also been applied to the program itself. Former and current staff said senior agency officials, aware of Trump’s denials of climate science, have tried to keep the program operating under the radar.
Self-censorship surfaced quickly after the 2016 election, even before Trump assumed office. In December of that year, the CDC environmental health director, Patrick Breysse, indefinitely postponed a first-ever climate symposium that was scheduled for after the inauguration. George Luber, then the CDC’s climate chief, remembers his superiors warning the event would be poorly timed; Breysse said the postponement was for budgetary reasons.
The environmental health chief acknowledges that his staff debated whether to use the term “climate change”. He later combined the climate and asthma programs and, internal documents suggest, omitted the word “climate” from the new branch’s title.
Breysse insists the White House never directed his actions. But they served as the basis for a whistleblower complaint filed by Luber, who was removed from his CDC post in 2018. The complaint alleged that Luber was ousted because of his outspokenness on global warming. It stirred a hornet’s nest of public attention, but some program insiders allege his removal had more to do with his mismanagement and mistreatment of employees than his advocacy.
The CDC, which refused to comment on “personnel matters”, said its climate program was running better than ever. The agency pointed to the “mini grants” it has doled out through partner organizations to help another 10 health departments, one-time funding of $5,000 to $50,000.
Meanwhile, every one of Trump’s budget proposals has tried to eliminate the program.
The inaction in Washington contrasts with some local efforts to save lives endangered by the climate crisis. In Phoenix, spurred on by the sustained surge in heat deaths, some groups hand out 250,000 bottles of water annually to the homeless. Others distribute heat awareness magnets and brochures to the elderly. Still others are developing home sensors that will notify friends and family when indoor temperatures climb.
Many vulnerable residents fall through the cracks. Arizona medical examiner records of heat deaths are filled with accounts of ageing and isolated people who hadn’t been heard from for days before a wellness check was requested.
Among them were Larry and Kathleen Purchase, 69 and 68 respectively, who died from environmental heat exposure in their Phoenix home during an unusual string of triple-digit days in September 2018. Married for almost 50 years, the two were active in their community and ran a small computer repair service, said Larry’s brother, Terry. When their 1970s rooftop air conditioner broke, they didn’t have the several hundred dollars to fix it.
Terry remembers them as “good stewards of the environment”, a tenet of their Christian faith. They didn’t believe in human-caused climate change, he said.
The day they were found, the temperature in their home hovered around 100F.
Dean Russell, Elisabeth Gawthrop, Veronica Penney, Ali Raj and Bridget Hickey are reporting fellows for Columbia Journalism Investigations, an investigative reporting unit at the Columbia Journalism School. Funding for CJI comes from the school’s Investigative Reporting Resource and the Energy Foundation. Additional support for this story was provided by the Fund for Investigative Journalism.
The Center for Public Integrity, a nonprofit investigative news organization, provided editing, fact checking and other support
Frieden, for his part, disputes claims that he did not prioritize climate change and insists he cares about the issue, pointing to the CDC’s work combating dangerous particulate matter produced by cars and coal plants. “It will have major public health consequences,” he said of climate change. “But there’s only a certain amount that public health programs can do.”
The CDC’s lackluster response contrasted with President Barack Obama’s public overtures and policy initiatives on climate. Former senior White House officials – including those who helped implement climate policies – admit the administration didn’t apply enough pressure on the CDC to act.
In December 2015, Republicans in Congress rejected a proposal to boost spending on the CDC program to $18m. The increase would have more than doubled its size.
When a broken air conditioner is lethal
The summer of 2016 – when Charlie Rhodes died – showed there was no time to lose in the push to understand and stem heat death. The previous eight years, the number of heat-related fatalities in Arizona had averaged 145. That jumped to 219 in 2016, and 264 the year after. A report produced by Maricopa county – where the largest number of the state’s heat deaths have occurred – found that men, Native Americans and people 75 and older were most at risk.
Gene Moore, 82, fit all three categories. A Quechan tribe member, he spent much of his life on its reservation, near Yuma, Arizona, before moving near Phoenix in 2010 to live with his son. Over the years, Moore’s health declined, but he remained mobile and enjoyed talking on the phone with friends, according to his son, Ivan.
In June 2017 – several weeks after Ivan had his home air conditioner repaired – he took his family camping in the mountains. Gene stayed behind. The day Ivan left, the temperature hit 118F. Phoenix went 11 days at or above 110F, one of only five such stretches on record. Four happened in the last three decades.
A week later, Ivan’s brother called to say Moore had stopped answering his phone. Ivan dialed the police. They found Moore dead on his bedroom floor, his window open. The air conditioner had broken again, and the temperature inside topped 105F. Moore’s autopsy shows cardiovascular disease caused his death, while heat played a significant contributing factor.
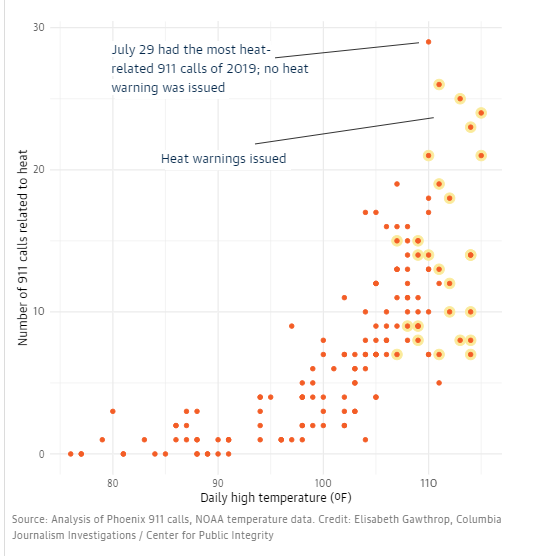
As the temperatures rise, so do calls for help
Phoenix’s summer of 2019 shows how hot the city already gets, and how heat-related 911 calls spike alongside the temperatures. The day with the most 911 calls hit 110 degrees without a heat warning issued.
Arizona health officials still don’t know why more residents like Moore are dying or how best to protect them. Temperatures are rising in the state, but the hottest summers don’t always match the highest death tolls. The Arizona State University researcher David Hondula, who works with the state’s climate team, contributed to a study ruling out temperature as the only reason. Other factors such as homelessness and substance abuse may play a role, he said, but the climate program doesn’t have money to keep studying the problem.
“If additional funding existed, we could really dive in to answer this question,” Hondula said. Instead, the limited CDC money – budgeted before the spike in deaths – supports awareness campaigns in poorer areas such as Yuma county.
Many Arizona cities offer cooling centers – air-conditioned libraries, churches and other shelters – for residents to escape the heat. Moore and Rhodes both had access to a vehicle. Cooling centers were nearby. Health workers are now surveying residents who visit cooling centers, but they say it takes money to determine why so many others don’t.
Ivan Moore, who grew up hearing about heat death victims on the radio, blames himself for what happened to his father. “I should have had someone check on him sooner,” Ivan said, even though less than 36 hours had passed between Gene’s last email to his family and when police found him. “He had quite a few years left on him.”
A worker collapse at a sweltering factory
In North Carolina, the CDC-funded program has helped enable what health department spokesperson Kelly Haight Connor described in an email as “the substantial growth in climate and health adaptation”. Even so, documents show the climate team ran into roadblocks almost as soon as it tried to evaluate the state’s preparedness for climate change. It was still seeking the agency’s assistance when, in 2015, it completed an analysis showing heat-related mortality would increase over the coming decade.
On 22 June that year, Sherion Winfrey, 63, had just returned to work after vacation and had nine days before she was due to retire. For nearly 40 years, she worked at the same oil- and air-filter factory in Fayetteville, North Carolina, a city in the Sandhills. She’d learned to pack frozen water bottles in a cooler to keep herself refreshed on the hot assembly line. But that day, as the temperature outside hit 96F, she collapsed during her shift. Rushed to a hospital, she died early that afternoon.
A state inspection of the factory the next day found that heat from industrial ovens and the metal walls and roof of the un-air-conditioned production line raised the indoor heat index – a combined measure of temperature and humidity – to over 106F and into the Occupational Safety and Health department’s “danger” heat classification. The inspector recommended the factory allow employees time to acclimate to the heat after an absence. But the investigation into Winfrey’s death ended after a medical examiner found that Winfrey suffered “a fatal pulmonary embolism and did not die from exposure to extreme temperatures”. Recent research suggests this type of blood clotting may be brought on by daily temperature swings.
Danny Muhammad, Winfrey’s son, has no doubt heat contributed to her death. Winfrey complained to family about the factory’s stifling environment. “The heat index was out of this world that day,” Muhammad said. It was the ninth consecutive day that temperatures had reached at least 94F – seven degrees hotter than the June average. Winfrey’s family filed a wrongful death lawsuit in 2017 against the factory, citing extreme indoor temperatures as the cause of her death, but the case was later dismissed. A spokesperson for the factory declined to comment.
It took another three years after Winfrey’s death for the North Carolina program’s heat education efforts to begin in four Sandhills counties – and not where she had lived.
Budget cuts and self-censorship under Trump
In the years since the Trump administration took over, the political pressure hampering some of the CDC climate program’s grantees has also been applied to the program itself. Former and current staff said senior agency officials, aware of Trump’s denials of climate science, have tried to keep the program operating under the radar.
Self-censorship surfaced quickly after the 2016 election, even before Trump assumed office. In December of that year, the CDC environmental health director, Patrick Breysse, indefinitely postponed a first-ever climate symposium that was scheduled for after the inauguration. George Luber, then the CDC’s climate chief, remembers his superiors warning the event would be poorly timed; Breysse said the postponement was for budgetary reasons.
The environmental health chief acknowledges that his staff debated whether to use the term “climate change”. He later combined the climate and asthma programs and, internal documents suggest, omitted the word “climate” from the new branch’s title.
Breysse insists the White House never directed his actions. But they served as the basis for a whistleblower complaint filed by Luber, who was removed from his CDC post in 2018. The complaint alleged that Luber was ousted because of his outspokenness on global warming. It stirred a hornet’s nest of public attention, but some program insiders allege his removal had more to do with his mismanagement and mistreatment of employees than his advocacy.
The CDC, which refused to comment on “personnel matters”, said its climate program was running better than ever. The agency pointed to the “mini grants” it has doled out through partner organizations to help another 10 health departments, one-time funding of $5,000 to $50,000.
Meanwhile, every one of Trump’s budget proposals has tried to eliminate the program.
The inaction in Washington contrasts with some local efforts to save lives endangered by the climate crisis. In Phoenix, spurred on by the sustained surge in heat deaths, some groups hand out 250,000 bottles of water annually to the homeless. Others distribute heat awareness magnets and brochures to the elderly. Still others are developing home sensors that will notify friends and family when indoor temperatures climb.
Many vulnerable residents fall through the cracks. Arizona medical examiner records of heat deaths are filled with accounts of ageing and isolated people who hadn’t been heard from for days before a wellness check was requested.
Among them were Larry and Kathleen Purchase, 69 and 68 respectively, who died from environmental heat exposure in their Phoenix home during an unusual string of triple-digit days in September 2018. Married for almost 50 years, the two were active in their community and ran a small computer repair service, said Larry’s brother, Terry. When their 1970s rooftop air conditioner broke, they didn’t have the several hundred dollars to fix it.
Terry remembers them as “good stewards of the environment”, a tenet of their Christian faith. They didn’t believe in human-caused climate change, he said.
The day they were found, the temperature in their home hovered around 100F.
Dean Russell, Elisabeth Gawthrop, Veronica Penney, Ali Raj and Bridget Hickey are reporting fellows for Columbia Journalism Investigations, an investigative reporting unit at the Columbia Journalism School. Funding for CJI comes from the school’s Investigative Reporting Resource and the Energy Foundation. Additional support for this story was provided by the Fund for Investigative Journalism.
The Center for Public Integrity, a nonprofit investigative news organization, provided editing, fact checking and other support
*Read the original article here
16 June 2020
The Guardian




